Uveitis
1. Uvéitis
Uveitis comprises a group of intra-ocular inflammatory diseases that can be purely inflammatory or in which inflammation is of infectious origin. The origin can take place in the retina or in the choroid or in both structures. It can also start from the shell of the eye, the sclera and is then called scleritis. Numerous causes, infectious or non-infectious, can be at the origin of the vast array of uveitis entities. This is a field in which the Centre for Ophthalmic Specialised care (COS) is a centre of excellence in the area but also receiving patients from beyond. Hereunder we describe a few examples of uveitis entities.
2. HLA-B27 uveitis (rheumatic uveitis)
HLA-B27 uveitis is the most frequently found type of uveitis under our latitudes. It is called such because it affects in close to 100% patients who have on the surface of their cells the human leucocyte antigen B27. These HLA antigens are present on the surface of all cells and determine the singularity of each individual. They are therefore responsible for graft rejection when transplantation is performed. HLA-B27 is present in about 7% of all individuals in Western Europe whereas it is very rare in Japan or other Asian countries with the corollary that this type of uveitis is rare in these countries.
It is an anterior non-granulomatous uveitis that can be associated with ankylosing spondylarthritis or not. Its course is usually acute or hyperacute presenting with a red eye without discharge of pus. It is almost always unilateral but during subsequent episodes it can involve randomly either eye (swinging uveitis). The patient should consult promptly as there is an exudation of proteins and inflammatory cells into the anterior chamber, into the aqueous humour. The inflammatory cells sediment on the interior surface of the cornea (the endothelium) as dust. Indeed, they never agglomerate as in herpetic anterior uveitis and the uveitis is therefore called non-granulomatous. It is consequently also impossible to have this dust deposit appear on photographs of the cornea. Proteins in the anterior chamber act as paste that sticks the iris posteriorly on the crystalline lens forming adherences (synechiae). If dilating drops (mydriatics) are not given rapidly the pupil remains stuck and cannot be dilated any more with a deformed pupil.
In a case of a hyperacute, unilateral non-granulomatous uveitis, the doctor should order an HLA-B27 test in the blood. About 60% of non-granulomatous uveitis are HLA-B27 positive and this rate is even higher when the uveitis is hyperacute. If the HLA-B27 antigen is found the diagnosis can be certain which is a relief for the doctor and the patient as the behaviour of the uveitis is known and its good prognosis can be anticipated. These HLA-B27 uveitis are known to present recurrences but each episode will respond to treatment. Therapy consists of the frequent administration of dilating drops to avoid synechiae and anti-inflammatory corticosteroid drops. At the beginning corticosteroid drops can be given as often as every 15 minutes and the frequency is then tapered over days and weeks. An episode usually lasts for about 3 weeks. In our centre we follow the inflammation very precisely using the laser flare photometry method. Recurrences can occur at any time interval. Therefore, the patient has to have an unopened bottle of corticosteroid and dilating drops each with him, as treatment has to be started as swiftly as possible, if a doctor cannot be consulted rapidly. In some cases, the patient may complain of articular lower back pain. He should then be referred to his family doctor or to the rheumatologist to investigate for ankylosing spondyarthritis.

3. Herpes Zoster Ophthalmicus (HZO) associated uveitis
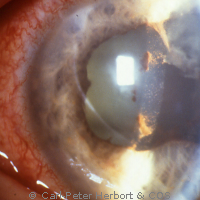
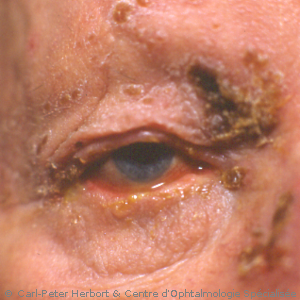
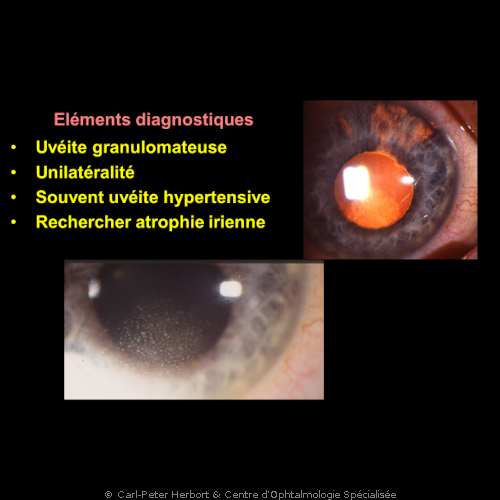
Ophthalmic herpes zoster (shingles) is produced by the varicella-zoster virus which is belonging to the family of herpes viruses. When individuals (children) are infected for the first time by this virus they develop varicella (chickenpox) characterised by a general outbreak of skin vesicles. The disease is very contagious. After this primoinfection the virus integrates many sensory nerve ganglions in an undetected latent form with only the hidden DNA present in the ganglion nerve cells. Shingles usually occurs in aged individuals or persons with a diminished immune system. In case of zoster ophthalmicus that involves the skin innervated by the first (superior, V1) division of the Vth cranial, there is a unilateral skin rash of the superior part of the head including the superior lid, the eye and the nose. Involvement of the conjunctiva and the corneal epithelium (zoster keratitis) as well as intraocular inflammation (zoster uveitis) can occur, very often causing areas of iris atrophy. Zoster uveitis often also causes an increase of intraocular pressure. The type of uveitis is granulomatous with medium-sized granulomatous KPs deposited on the interior surface of the cornea. Because of such possible ocular complications all cases of ophthalmic zoster have to get an immediate eye check-up. To avoid long-term severe complications, systemic (oral) antiviral tablets (valganciclovir, 3X 1000 mg) have to be given within 3 days of the initial symptoms. At the ocular level, treatment consists of antiviral ointment for the keratitis and the uveitis. Topical corticosteroid drops have to be given in addition to antiviral therapy, when uveitis is detected. This type of uveitis can become chronic and needs constant follow-up and prolonged antiviral and topical corticosteroid treatment. More often than herpes keratitis, there are subepithelial nummular scars that can be limited by prolonged corticosteroid drop treatment.
4. Herpes simplex uveitis (herpetic uveitis)
Herpes simplex virus can cause superficial disease when it involves the corneal epithelium (dendritic keratitis) but it can also involve more deep structures like the corneal stroma (stromal keratititis) or the inside of the eye (herpes uveitis). When both these structures are touched, we speak of herpetic keratouveitis. The uveitis is of the granulomatous type with well-identifiable KPs deposited on the interior surface of the cornea which is distinguishing it clearly from HLA-B27 uveitis where deposits on the interior surface of the cornea are no more than dust. The uveitis is unilateral and recurrences always occur on the same side. It very often causes ocular hypertension and iris atrophy. Its treatment consists in antiviral tablets (valganciclovir 3 X 500 mg) together with local ocular antiviral ointment associated with corticosteroid drops. When the pressure is increased, pressure-lowering drops have to be given.
5. Fuchs’ uveitis
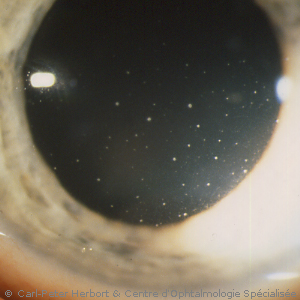
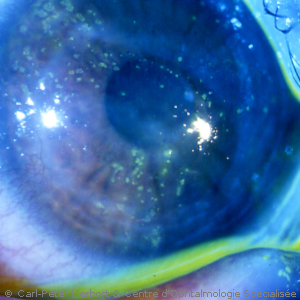
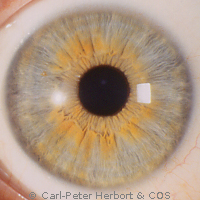
This uveitis has been described for the first time by Ernst Fuchs in 1906, a professor of ophthalmology in the University of Vienna who gave his eponym (name) to this particular inflammatory eye condition. The particularity of this uveitis, unilateral in 9 out of 10 cases, is the difference of colour between the two irises, the diseased eye being the lighter coloured eye. However, when the iris colour is brown, no heterochromia is seen but a difference of structure of the iris is always present. Two more important clinical signs are the fine micro-granulomatous deposits on the inner surface of the cornea (keratic precipitates, KPs) easily identifiable, the sign of a granulomatous uveitis. In some areas (North America) the uveitis is falsely considered as non-granulomatous. Another characteristic finding present in 100% of cases is the infiltration of the vitreous gel by inflammatory cells (vitritis).
It is the uveitis with the most often missed diagnosis and/or which is diagnosed with a substantial delay because the doctor is looking for heterochromia which is absent in brown irises. This has often dramatic consequences, as the condition does not respond to anti-inflammatory treatment, leading the doctor to prescribe oral, systemic treatment with their deleterious side-effects when no treatment is necessary.
No treatment is efficacious and, in fact, no treatment is necessary. It is crucial to avoid to give corticosteroid drops that can only make things worse by accelerating cataract formation and by potentially causing an increase of the intraocular pressure. However, it is necessary to follow these patients once yearly to monitor the development of a cataract or the occurrence of an increase of intraocular and the development of glaucoma.

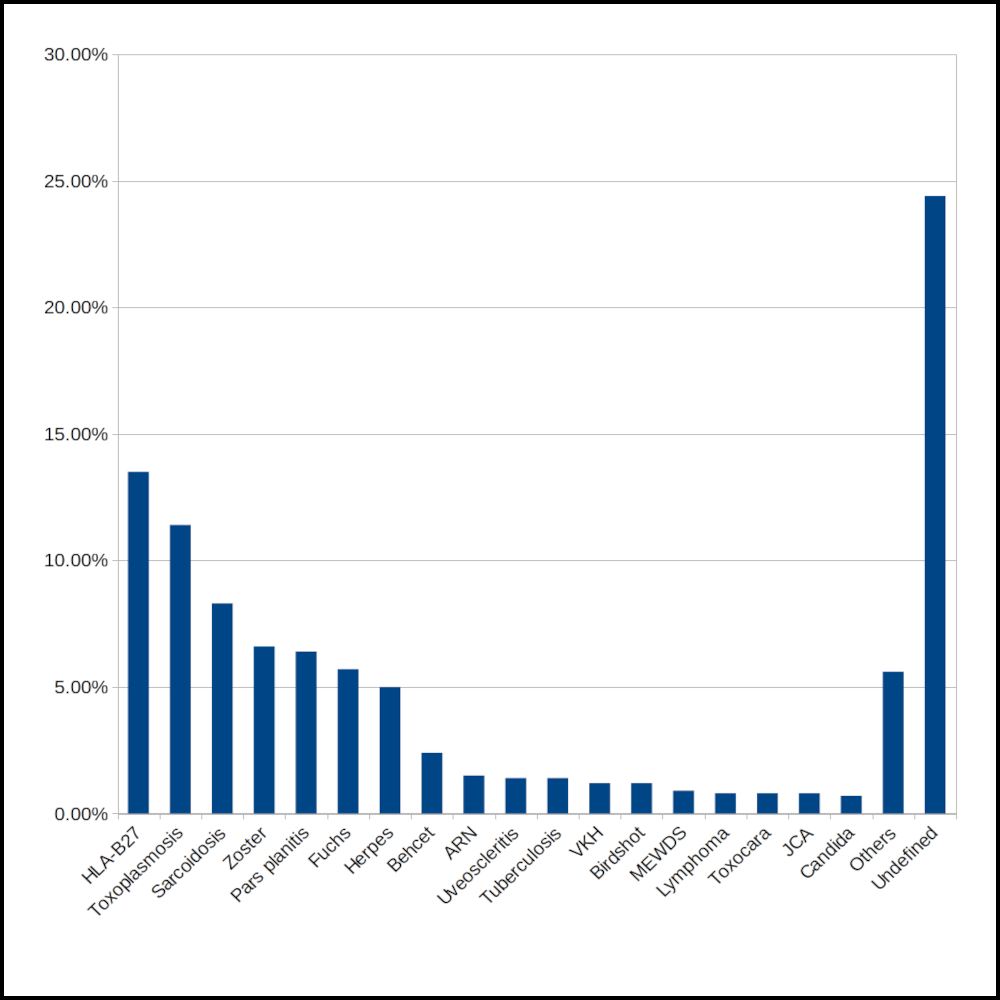
6. Uvéites en Suisse romande
During the 1990ties we performed an epidemiological study never performed before looking at the type of uveitis entities and their frequencies occurring in our area, the French speaking part of Switzerland. By far the two types of uveitis entities most frequently occurring in our area is HLA-B27 related uveitis and toxoplasmic uveitis followed by uveitis related to herpes zoster ocular infection and to ocular herpes simplex infection, as well as Fuchs’ uveitis. A detailed classification and frequency of uveitis is shown on the figure.